Advertisment
Researchers develop clinically validated, wearable ultrasound patch for continuous blood pressure monitoring
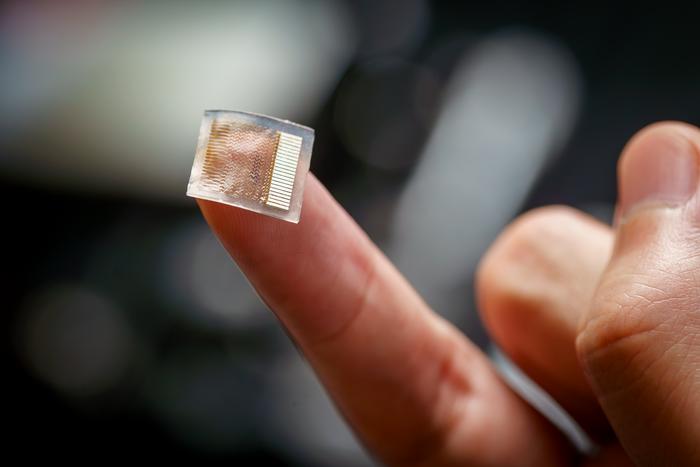
A team of researchers at the University of California San Diego has developed a new and improved wearable ultrasound patch for continuous and noninvasive blood pressure monitoring. Their work marks a major milestone, as the device is the first wearable ultrasound blood pressure sensor to undergo rigorous and comprehensive clinical validation on over 100 patients.
The technology, published on Nov. 20 in Nature Biomedical Engineering, has the potential to improve the quality of cardiovascular health monitoring in the clinic and at home.
“Traditional blood pressure measurements with a cuff, which are limited to providing one-time blood pressure values, can miss critical patterns. Our wearable patch offers a continuous stream of blood pressure waveform data, allowing it to reveal detailed trends in blood pressure fluctuations,” said study co-first author Sai Zhou, who recently graduated with his Ph.D. in materials science and engineering from the UC San Diego Jacobs School of Engineering.
The patch is a soft and stretchy device, about the size of a postage stamp, that adheres to the skin. When worn on the forearm, it offers precise, real-time readings of blood pressure deep within the body. The patch is made of a silicone elastomer that houses an array of small piezoelectric transducers sandwiched between stretchable copper electrodes. The transducers transmit and receive ultrasound waves that track changes in the diameter of blood vessels, which are then converted into blood pressure values.
Technological improvements to wearable ultrasound
The wearable ultrasound patch builds upon an earlier prototype that was pioneered by the lab of Sheng Xu, a professor in the Aiiso Yufeng Li Family Department of Chemical and Nano Engineering at UC San Diego. Researchers re-engineered the patch with two key improvements to enhance its performance for continuous blood pressure monitoring. First, they packed the piezoelectric transducers closer together, enabling them to provide wider coverage so they could better target smaller arteries such as the brachial and radial arteries, which are more clinically relevant. Second, they added a backing layer to dampen redundant vibrations from the transducers, resulting in improved signal clarity and tracking accuracy of arterial walls.
In tests, the device produced comparable results to a blood pressure cuff and another clinical device called an arterial line, which is a sensor inserted into an artery to continuously monitor blood pressure. While the arterial line is the gold standard for blood pressure measurement in intensive care units and operating rooms, it is highly invasive, limits patient mobility, and can cause pain or discomfort. The patch provides a simpler and more reliable alternative, as shown in validation tests conducted on patients undergoing arterial line procedures in cardiac catheterization laboratories and intensive care units.
Comprehensive clinical validation
Researchers conducted extensive tests to validate the patch’s safety and accuracy. A total of 117 subjects participated in studies that evaluated blood pressure across a wide range of activities and settings. In one set of tests, seven participants wore the patch during daily activities such as cycling, raising an arm or leg, performing mental arithmetic, meditating, eating meals and consuming energy drinks. In a larger cohort of 85 subjects, the patch was tested during changes in posture, such as transitioning from sitting to standing. Results from the patch closely matched those from blood pressure cuffs in all tests.
The patch’s ability to continuously monitor blood pressure was evaluated in 21 patients in a cardiac catheterization laboratory and four patients who were admitted to the intensive care unit after surgery. Measurements from the patch agreed closely with results from the arterial line, showcasing its potential as a noninvasive alternative.
“A big advance of this work is how thoroughly we validated this technology, thanks to the work of our medical collaborators,” said Xu. “Blood pressure can be all over the place depending on factors like white coat syndrome, masked hypertension, daily activities or use of medication, which makes it tricky to get an accurate diagnosis or manage treatment. That’s why it was so important for us to test this device in a wide variety of real-world and clinical settings. Many studies on wearable devices skip these steps during development, but we made sure to cover it all.”
Next steps
The research team is preparing for large-scale clinical trials and plans to integrate machine learning to further improve the device’s capabilities. Efforts are also underway to validate a wireless, battery-powered version for long-term use and seamless integration with existing hospital systems.
Paper: “Clinical validation of a wearable ultrasound blood pressure sensor.” Co-authors include Sai Zhou*, Geonho Park*, Katherine Longardner*, Muyang Lin*, Baiyan Qi, Xinyi Yang, Xiaoxiang Gao, Hao Huang, Xiangjun Chen, Yizhou Bian, Hongjie Hu, Ray S. Wu, Wentong Yue, Mohan Li, Chengchengfang Lu, Ruotao Wang, Siyu Qin, Isac Thomas, Benjamin Smarr, Erik B. Kistler, Belal Al Khiami, Irene Litvan and Sheng Xu, UC San Diego; and Esra Tasali and Theodore Karrison, The University of Chicago.
*These authors contributed equally to this work.
This work was supported by a Wellcome Trust Innovator Award (WT215841/Z/19/Z) and the National Institutes of Health (1 R01 EB3346401).
All bio-experiments were conducted in accordance with the ethical guidelines of the National Institutes of Health and with the approval of the Institutional Review Boards of the University of California San Diego.
Image: This small, stretchy skin patch uses ultrasound to continuously monitor blood pressure deep inside the body. A comprehensive clinical validation on 117 subjects, including patients in the intensive care unit, has demonstrated its potential as a simpler and more reliable alternative to current clinical methods for monitoring blood pressure.
View more Credit: David Baillot/UC San Diego Jacobs School of Engineering