Advertisment
Drug for panic disorder less effective than previously believed
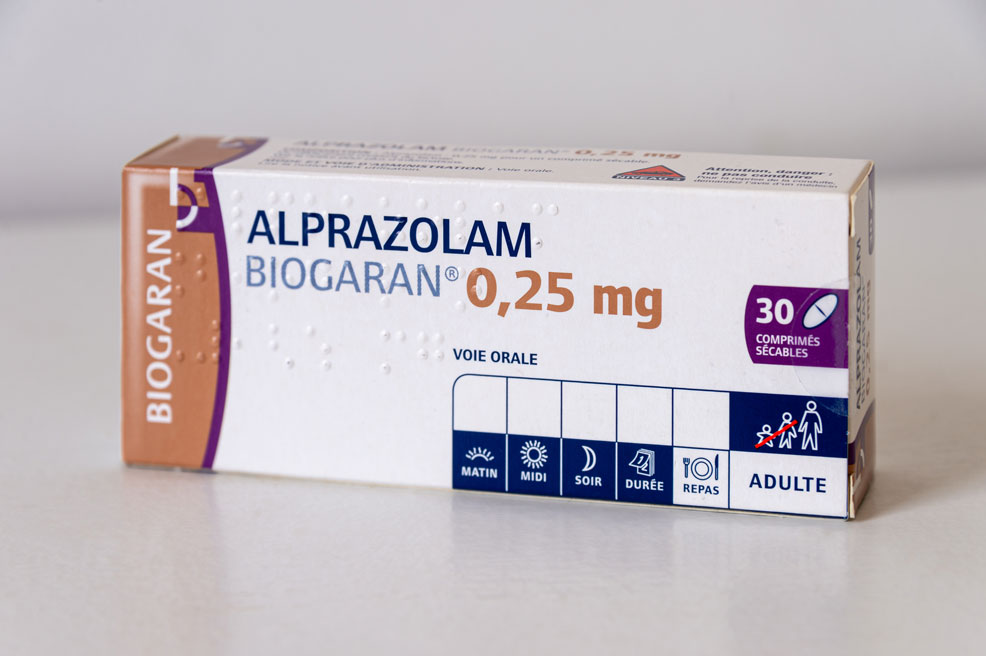
New research reveals that the nation’s most widely prescribed type of sedative may be less effective than clinicians and scientists have been led to believe, based on publications in medical journals.
The study, which published today in the journal Psychological Medicine, examined both published and unpublished data from five randomized controlled clinical trials reviewed by the Food and Drug Administration for alprazolam, known by the trade name Xanax XR. It is one of a class of sedatives known as benzodiazepines, widely prescribed since the 1970s to treat medical conditions such as anxiety and insomnia.
In recent years, benzodiazepines have been associated with serious clinical risks, including dependence, withdrawal, falls and cognitive impairment.
“Clinicians are well aware of these safety issues, but there’s been essentially no questioning of their effectiveness,” said senior author Erick Turner, M.D., professor of psychiatry at the Oregon Health & Science University School of Medicine and former FDA reviewer. “Our study throws some cold water on the efficacy of this drug. It shows it may be less effective than people have assumed.”
Turner and co-author Rosa Ahn-Horst, M.D., M.P.H., a resident in psychiatry at Harvard University, reviewed publicly available FDA data from phase 2 and phase 3 clinical trials conducted for extended-release alprazolam for the treatment of panic disorder. The extended-release formulation was approved by the FDA in 2003, while the original immediate-release formulation was approved in 1981.
They found that five trials had been conducted, but only three of them had been published in medical journals. Further, when the FDA reviewed the drug company’s trial results on how well the drug performed compared with a placebo, Turner said they determined that only one of the five trials had a clearly positive outcome.
Using meta-analysis, a statistical method of combining all study results, they found that alprazolam extended-release was still superior to a placebo, but not as much as the published data had conveyed. Specifically, they found that publication bias inflated the drug’s efficacy by more than 40%.
Turner said the findings may be especially relevant to patients and clinicians who haven’t used benzodiazepines previously, as opposed to those who use the drug infrequently or who have already become physically dependent.
“This study will reinforce being cautious about starting a prescription,” Turner said.