Advertisment
Home testing kits and coordinated outreach substantially improve colorectal cancer screening rates
Colorectal cancer screening is an effective tool for catching the disease early when it’s most treatable, yet it is underutilized in patient populations who receive primary care at federally qualified health centers (FQHC).
A new study by researchers at UNC Lineberger Comprehensive Cancer Center demonstrated that a targeted intervention can substantially increase screening rates in patients who are not current with recommended screening. The researchers report in JAMA Network Open that mailing at-home colorectal cancer screening kits and providing coordinated follow-up led by an academic cancer center tripled screening completion rates compared to usual care at FQHCs.
Previous research has shown this kind of intervention is effective in large, integrated health systems. However, its impact was unknown in FQHCs, which operate as small, grant-funded entities that are often under-resourced and serve as safety-net care providers. Daniel Reuland, MD, MPH, the study’s corresponding author, said increasing the screening rate at FQHCs, which provide care to 1 in 11 people in the United States, could reduce the rate of colorectal cancer incidence and death and improve the care of many underserved populations.
“Reaching a largely unscreened, predominantly low-income population using centralized mailed screening kits and patient navigation for those with abnormal tests can substantially increase guideline-recommended colorectal cancer screening in federally qualified health centers,” said Reuland, the Robert A. Ingram Distinguished Professor at UNC School of Medicine and co-director of the UNC Lineberger Carolina Cancer Screening Initiative (CCSI).
This is especially true with North Carolina’s community health centers, which serve patient populations and communities that have low colorectal cancer screening rates. Reuland said many individuals in these communities have never been screened.
The National Cancer Institute estimates that more than 152,000 people in the U.S. will be diagnosed with colorectal cancer this year, and the disease will cause approximately 53,000 deaths. While rates have declined in people 65 and older, cases and deaths among those under 50 have been rising since 1990.
The new study, called Scaling Colorectal Cancer Screening through Outreach, Referral and Engagement, or SCORE, was conducted in partnership with two FQHCs in North Carolina: Blue Ridge Health, based in Hendersonville and Roanoke Chowan Community Health Center in Ahoskie. It enrolled 4,002 participants aged 50 to 75 who had an average colorectal cancer risk and were not current with recommended screening guidelines.
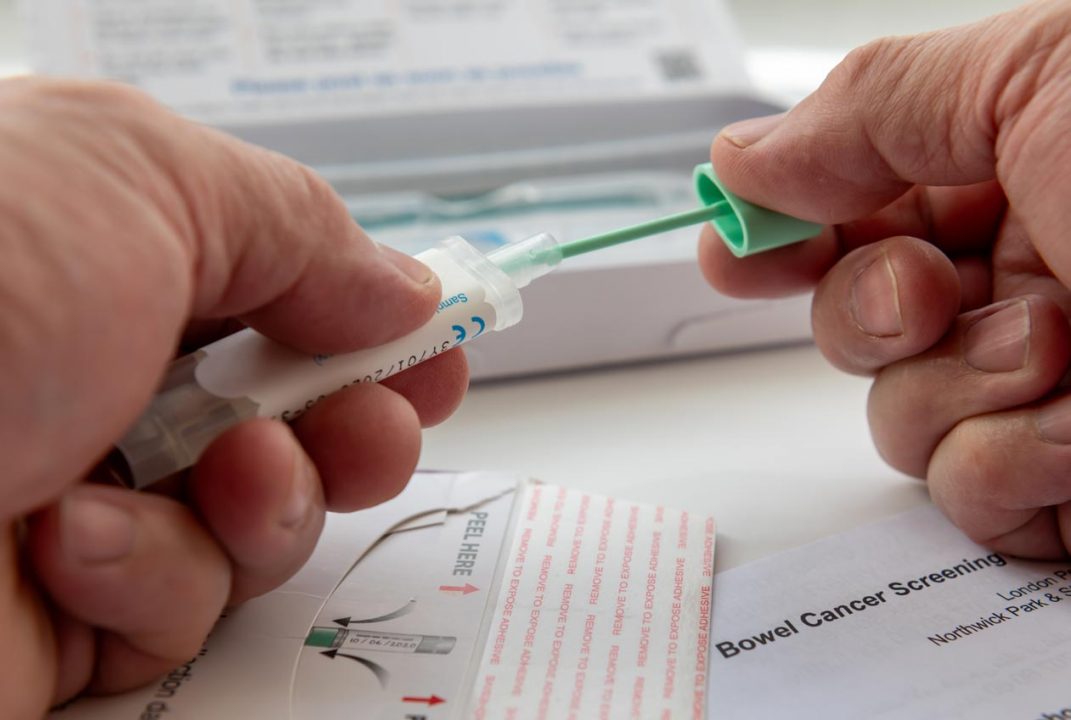
Half of the participants were enrolled in the intervention arm. In addition to receiving usual care, they were mailed a free, at-home fecal immunochemical testing (FIT) kit and provided navigation services for follow-up colonoscopies if the at-home FIT was positive. A positive test result indicates there was trace amounts of blood in the stool, which could be an early sign of cancer. The other half received usual care alone.
The study aimed to measure how many participants would complete a colorectal cancer screening within six months and how many would undergo a colonoscopy within six months following a positive FIT result. In collaboration with the FQHC staff, the CCSI outreach team distributed the FIT kits and coordinated result tracking and follow up on positive FIT results. the navigator ensured the information was entered into the participants’ electronic health records and communicated with their primary care providers.
The study found that participants in the intervention group were three times more likely to be screened within six months (30% vs. 9.7%). By 12 months, screening completion rates increased to 34.6% in the intervention group and 16.6% in the control group.
Among those who had a positive FIT result, the intervention group had a higher follow-up colonoscopy rate, with 68.8% completing the procedure compared to 44.4% in the control group.
“Mailed FIT is an excellent complement to usual care screening services,” said paper coauthor Alison Brenner, PhD, MPH, CCSI deputy director and associate professor at UNC School of Medicine. “It reaches a lot of patients who, for whatever reason, aren’t getting screened in usual care and significantly increases screening rates. A centralized approach, like the SCORE trial demonstrated, can relieve both the under-resourced FQHCs as well as the over-packed agenda of primary care by taking care of this preventive service outside of the clinic visit.”
Based on these findings, the researchers are investigating how to expand the program.
“Our team is completing a cost analysis of the intervention. FIT testing is inexpensive, so we anticipate that this kind of outreach will be a very cost-effective way to improve population screening. In tandem with this, we’re working to find ways to scale and sustain this kind of intervention to have greater impact,” Reuland said.
This includes having preliminary conversations with officials with North Carolina Medicaid, which expanded eligibility last year to cover more people.
“There is limited colonoscopy capacity in many parts of North Carolina, and with the Medicaid expansion, the need for colonoscopies is increased,” Reuland said. “This kind of FIT-based outreach strategy could help us increase screening while making optimal use of limited colonoscopy capacity.”
Authors and Disclosures
The research was supported by the National Cancer Institute and the University Cancer Research Fund and gifts from John Goodacre and Donna and Greg Schmidt.
A comprehensive listing of the authors and any potential conflicts of interest can be found in the full publication of this research.